The Centers for Medicare and Medicaid Services (CMS) released the 2022 Medicare Physician Fee Schedule (PFS) in early July 2021. Major cuts were proposed for peripheral arterial disease (PAD) reimbursement in the office-based laboratory (OBL). If these proposed rates become finalized, there will be approximately a 20% reduction in
reimbursement for PAD cases performed in the OBL, which will close the gap between OBL and ambulatory surgical center (ASC) reimbursement for PAD. Dramatic fee cuts for PAD in the OBL were proposed in 2014 and 2018, but neither fee cut was ultimately finalized. Will this proposed cut for PAD reimbursement in the OBL be approved
for 2022? We must wait until November 2021 for the Final Fee Schedule (FFS) to find out.
PAD in the OBL dodged the reimbursement reduction bullet in 2021, because Congress intervened and
overturned the Medicare FFS 8-10% reimbursement reduction for PAD in the OBL with the CARES Act
Provider Relief Fund-H.R. 8702 (116th).
PAD reimbursement rates in the OBL have remained relatively unchanged from 2008-2021, while the price of equipment, specifically, atherectomy tools, has dropped significantly through aggressive pricing programs like bundling, bulking, and rebates from the vendors. Due to the regulations and costs to build and operate an ASC, it is typical for procedures to reimburse at much higher rates in an ASC than an OBL — PAD is one of the rare exceptions. Currently, PAD reimbursement rates are higher in an OBL than an ASC and when the 2022 FFS is announced in November 2021, we will see whether this reimbursement anomaly continues. Both sites of service (OBL and ASC) are dramatically less expensive than the Hospital Outpatient Department (HOPD) rates.
Thank the Cardiovascular Coalition
The Cardiovascular Coalition’s (CVC) focus is to advance patient access to care for PAD. This coalition is comprised of physicians, care providers, advocates, and device manufacturers. The CVC
was instrumental in leading the efforts to roll back significant proposed PAD reimbursement cuts (30-50%) in the OBL in 2014 and 2019, helped establish the first-ever PAD Caucus in 2019, and recently re-introduced the Amputation Reduction and Compassion (ARC) Act (H.R. 2631), available online at ttps://cardiovascularcoalition.com/the-amputation-reduction-and-compassion-arc-act/.
If you are in the process of developing an office-based lab (OBL), consider mitigating your risk by designing it with a comprehensive strategy to convert to an ambulatory surgical center (ASC).
The ARC Act provides coverage of PAD screening for at-risk beneficiaries under the Medicare and Medicaid programs without the imposition of cost-sharing requirements, and disallows payments for amputations unless patients have had anatomical testing 3 months prior to amputation.
In 2018, the CVC was successful in overturning limited coverage decisions in 10 states that would have prevented lower-extremity revascularization procedures in the OBL site of service. Without CVC’s efforts and representation in Washington, D.C., the current reimbursement in the OBLs would look dramatically different.
How CPT Procedure Codes are Valued: Rationale for Code Change
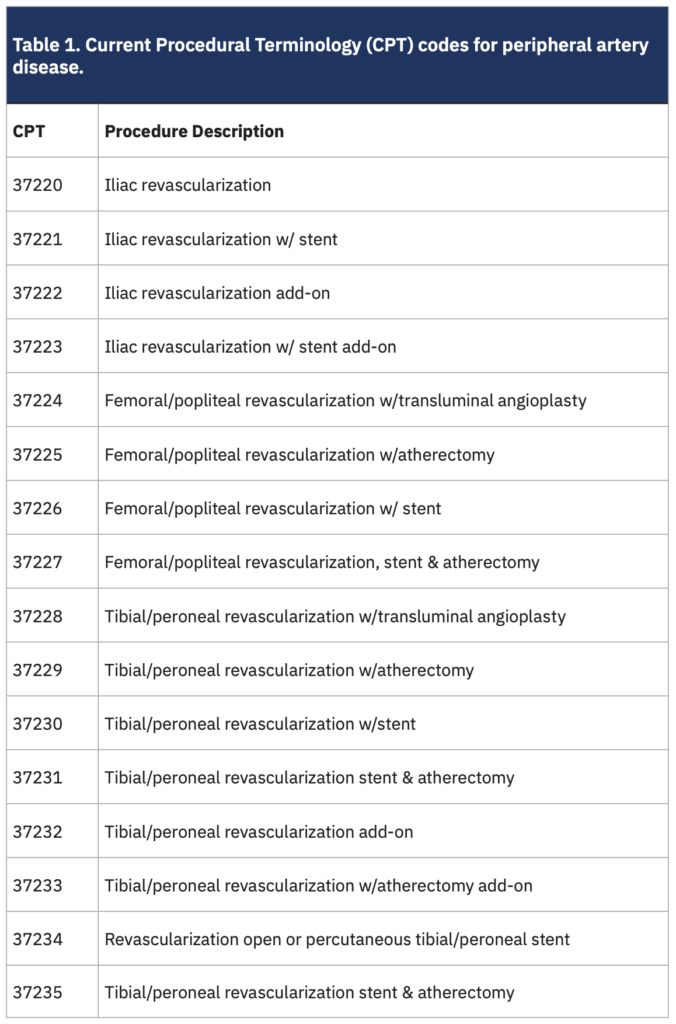
The American Medical Association (AMA) reviews and evaluates all Current Procedural Terminology (CPT) code change applications via the CPT/ Primary Care Physicians Advisory Committee (PCPAC) and the CPT Editorial Panel. The RVS Update Committee (RUC) is an AMA multispecialty committee that provides medicine a voice in shaping Medicare rates; the RUC provides recommendations, but CMS ultimately makes all final decisions on Medicare payments. The RUC is currently reviewing endovascular revascularization (application a602239 was submitted June 29, 2020). This review had no impact on the proposed 20% cut for 2022. The RUC noted that CPT code 37229 (Table 1) was identified on the high-volume growth screen at this meeting and agreed with the specialty societies’ suggestion to refer this entire family of PAD CPT codes in order to revise the descriptors and accommodate new technologies.
CPT codes 37225, 37227, and 37229 (Table 1) were identified as procedures with high-cost supplies in OBLs that have not been reviewed in the last five years and include a supply item greater than $500. Code 37229 was also identified as a high-growth procedure in the OBL, since usage has increased by at least 100% from 2012 through 2017. The stakeholder societies (Society of Vascular Surgeons [SVS], Radiologic Society of North America [RSNA], and Society of Interventional Radiology [SIR]) commented:
“We believe the growth in CPT Code 37229 is appropriate and in line with the best practices for limb sparing. However, there have been many advances in lower extremity endovascular treatment since the creation of this family of codes. The specialties recommend referring this set of codes to CPT to update the code descriptors and to accommodate new technologies.”
The stakeholder societies submitted an Action Plan in January 2019 that added codes 37220 to 37235 as a family of codes. CMS conducted in-depth market research to update the PFS for supply and equipment pricing, and have adjusted the price to market value for ‘high-cost supply’ items.
This code change application proposes to differentiate and describe precise anatomic reporting of procedures through a series of primary procedures and a series of add-on codes in order to reflect the work and the practice expense of commonly applied technologies. The group is proposing deleting 16 CPT codes (3722 to 37235), and creating 24 primary anatomic codes and 7 add-on technology codes. What does this mean for overall PAD reimbursement in the OBL? It may end up looking like fistula maintenance OBL reimbursement cuts in 2017.
Will History Repeat Itself?
In 2017, CMS bundled the fistula maintenance CPT codes, which translated to a ~40% reduction in OBL reimbursement while leaving the rates relatively unchanged in the ASC site of service. The Society of Diagnostic and Interventional Nephrology stated that nearly 20% of the freestanding vascular access centers (VACs) closed since the new codes were created.2 What if 2022 proposed fee schedule’s 20% cut is finalized? What if in 2023 the AMA’s proposed new anatomic codes for PAD in the OBL result in additional reimbursement reductions and the result is similar to how fistula maintenance procedures were affected in 2017? How many of the 600-700 endovascular OBLs in the United States could survive?
Lessons Learned from the Vascular Access Center (VAC) Reimbursement Reduction
- Understand trends and changes in Medicare reimbursement
- Engage ASC representation in Washington, D.C., to protect your investment by joining the Cardiovascular Coalition (CVC).
- If you are in the process of developing an OBL, consider mitigating your risk by designing it with a comprehensive strategy to convert to an ASC.
- When rates change in the OBL, you will be able to quickly pivot to an ASC and expand to procedures such as electrophysiology (EP) implants, as well as recent additions such as diagnostic catheterizations and percutaneous coronary intervention.
- If you currently own an OBL, consider engaging an ASC development or consulting firm for a feasibility assessment study to understand what options you have if rates change.
- Understand your exit strategies if your OBL is not easily convertible to an ASC.
- Consider alignment with other subspecialties:
- Interventional radiology
- Interventional nephrology
- Radiology oncology
- Vascular surgeons
Conclusion
Building an endovascular OBL today may be shortsighted. The reimbursement has run its course for 12 years and, like most procedures that shift to the outpatient setting, will eventually see a leveling off. Developing an ASC is a daunting task, and the risks and benefits should be thoroughly evaluated. Developing and managing an ASC independently could alienate referral sources and strain relationships with local health systems, both of which could have long-term negative consequences. It may make sense to keep an open mind regarding joint venture partnership options, which decrease risk and increase opportunities, rates, efficiencies — and exit strategies. n References 1. Code Change Application a602329, updated June 29, 2020. CPT is a registered trademark of the American Medical Association. 2. Litchfield T. Dialysis access coding essentials, recent changes, and location distinctions. Endovascular Today. June 2019. Accessed July 20, 2021. Available online at https://evtoday.com/articles/2019-june/dialysis-access-coding-essentials-recent-changes-and-location-distinctions
References
- Code Change Application a602329, updated June 29,
- CPT is a registered trademark of the American
Medical Association. - Litchfield T. Dialysis access coding essentials, recent
changes, and location distinctions. Endovascular Today.
June 2019. Accessed July 20, 2021. Available online
at https://evtoday.com/articles/2019-june/dialysis-access-coding-essentials-recent-changes-and-location-distinctions
Note: This article was also shared on MedAxiom, an ACC Company,
at https://www.medaxiom.com/news/2021/07/15/partner-news/
the-9-lives-of-pad-reimbursement-in-the-obl



